Ganglia of the Hand and Wrist
A ganglion cyst is a tissue sac filled with a very thick, jelly-like material. It is usually painless, however when it does become painful, it may be a sign of rapid growth or pressure on a nearby nerve. Ganglia are the most common soft tissue growths of the hand and wrist, representing about 50-70% of all tumors in this area of the body.
Some patients may choose to leave smaller, non-painful ganglia untreated. However when a ganglion cyst becomes large and painful or if it is located in the wrist, surgical treatment may be the best course of action.
Learn more about ganglia below, or contact us today to schedule an appointment for your ganglion cyst evaluation.
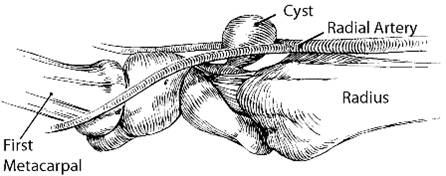
Diagram of a wrist ganglion cyst (as seen from the side with the wrist turned palm upwards)
Introduction
A ganglion cyst is usually solitary and may arise from anywhere in the wrist and hand. The most common sites are probably the top of the wrist at its midline, palmar wrist along the thumb side, and the end joints of the fingers at the distal interphalangeal joint.
Ganglia can occur at any age but are most prevalent between age 10 and 40, including childhood. Interestingly, as with many other illnesses, they affect women about 3 times more often than men. The right and left hands are affected with equal frequency. There has been no evidence of racial predisposition identified and no occupation has been specifically identified as likely to precipitate development of a ganglion cyst.

Causation
Ganglia develop from the connective tissue by liquefaction (decay) of collagen fibers, increasing the amount of fluid. Though many of the ganglia arise directly adjacent to a joint, they appear to be connected by a one-way valve mechanism allowing fluid from the joint to exit into the sac.
Ganglia may arise adjacent to a joint or tendon sheath and may be connected by a long stalk. Thus, their superficial appearance may not accurately represent the site of origin. Ganglia arising in response to degenerative arthritis of the interphalangeal joint are called mucous cysts and frequently result in deformity of the fingernail. If they go untreated and rupture, they may become infected. Ganglia cysts commonly occur in association with arthritis related to production of inflammatory fluid.
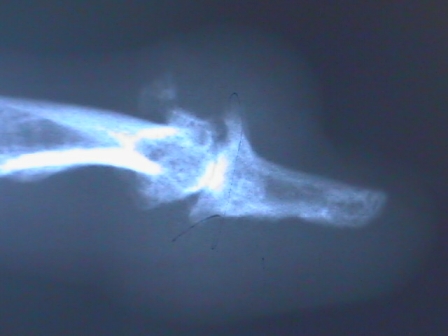
Advanced degenerative arthritis at the end joint of the finger (DIP joint) frequently results in a cyst known as a mucous cyst and may cause significant nail deformity.

Cyst caused by arthritis

Cyst at nail fold that has popped

Pressure from a cyst just above the nail fold has caused a deep trough in the nail. Removal of the cyst will allow the nail to grow back normally in about 4 months.
WARNING: MAY CONTAIN GRAPHIC IMAGES
Symptoms
A wrist ganglion may produce pain and associated weakness, or present as a painless lump. Wrist ganglia may occur in association with ligamentous instability about the wrist. However, that is not a common finding. Ganglia may be noticed suddenly with or without pain. The majority probably develop slowly over a period of months. Spontaneous disappearance of ganglia has been reported in up to 58% of patients in some series.
Differential Diagnosis
It is not unusual to have a person come in with a ganglion thinking that it's causing the symptom of pain in the hand or wrist, when in fact the ganglion has probably been present all along and it is not really causing any discomfort. Associated problems such as de Quervain's tendonitis or carpal tunnel syndrome can cause the symptoms, thus drawing attention to the lump. (the alternatives, which may be considered as possible explanations appearing in a similar fashion to ganglia.)
Evaluation
Most ganglia are obvious because of the classic location, size and symptoms. Physical examination is sufficient in making a diagnosis. A ganglion is usually not mobile and it frequently has bounce to touch. However, in an attempt to identify an underlying cause such as arthritis and exclude other explanations, X-rays may be necessary.
Non-Operative Treatment
A person who notes a lump but is not experiencing pain or limitation as a result of the lump has choices. She may observe the lump and do nothing. The lump may be struck to try and pop it in hope that it scars down and does not recur. This is unpredictable. The other option is surgical removal (excisional biopsy). If the lump is large enough to be ugly or is bothersome it may need to be removed surgically.
An attempt at withdrawing the jelly-like fluid from the ganglion with a needle is largely unsuccessful; usually the cyst will recur. Some physicians have reported good results from cortisone injection, but in my experience there is a high recurrence rate after injection. There is no good physiological reason why corticosteroids should have any effect on this problem.
Surgical Treatment
Ganglia arising directly off the pulley holding the flexor tendon in place (flexor retinacular cysts), are usually uncomfortable, interfere with grip, and usually require surgical excision. Increased discomfort can occur on ring fingers because of pressure from the ring on the mass and the adjacent digital nerve.
In the case of mucus cysts involving the finger or thumb distal interphalangeal joint, it's necessary to remove osteophytes (bone) from the underlying joint in addition to the soft tissue sac. A small 1/2" incision is made to remove the cyst. The semi-line prevents the scar from pulling tightly across the finger. Nail deformity coming from pressure against the growth area will then correct itself as the nail regrows.

Example of a mucous cyst

Nail deformity from a mucous cyst
Traditional Surgery (Wrist Ganglion):
Ganglion removal is best done using a small 1/2" transverse incision. The ganglion is exposed down to the joint and cut out along with a small wedge of the joint capsule.
Arthroscopic Surgery:
There is an arthroscopic technique for removing a wrist ganglion. It is straightforward and requires two small puncture wounds in the wrist. It is as equally effective as open ganglion removal only it leaves an even smaller incisional scar and it costs a lot more due to use of elaborate equipment. For the person determined to absolutely minimize the size of the scar and for whom "money is no object" - there aren't many of those around - arthroscopic removal of a ganglion is a safe, straightforward outpatient procedure. Surgical removal of ganglia in general is quite effective. However, in order to obtain a good result one must do the surgery in an operating room. This prevents injury to associated structures such as the superficial nerves and arteries and minimizes incision size. It decreases the chance of recurrence by allowing careful dissection down to the base of the ganglion and excision of the entire ganglion with its origin.
Physical or Occupational Therapy
It's rare for a person who undergoes ganglion removal to require hand therapy afterwards if treated at Nebraska Hand & Shoulder Institute, P.C. There is usually minimal discomfort after surgery. Since there are no restrictions necessary, the patient is allowed to move her fingers and wrist immediately. Significant stiffness develops only if the patient babies herself and refuses to do simple exercises. Total ganglion removal provides 85-90% chance of permanent cure. Surgery achieves difinitive tissue diagnosis and treatment in one sitting. If the specimen appears classical for a benign (non cancerous) ganglion, it may not be necessary to send it to a pathologist and incur an additional charge, though hospital regulations may mandate having the pathologist look at the specimen. Having an absolute tissue diagnosis often provides an unparalleled measure of confidence in a person by eliminating the fear of an undiagnosed cancer.
Barnes WE, Larson RD, Posch JL: Review of ganglia of the hand and wrist with analysis of surgical treatment. Plastic and Reconstructive Surgery 1964;34:570-574.
Boyes JH. Surgery of the Hand. Philadelphia: Lippicott JB. 1970;5:669
Eaton RG, Dobranski AI, Littler JW: Marginal osteophyte excision in treatment of mucous cysts. J Bone Joint Surg Am 1973;55:570-574.
Flynn JE. Hand Surgery. Baltimore. Williams and Wilkins. 1982:898-902.
Gingrass MK, Brown RE, Zook EG: Treatment of fingernail deformities secondary to ganglions of the distal interphalangeal joint. J Hand Surg [Am] 1995;20:502-505.
Gunther SF: Dorsal wrist pain and the occult scapholunate ganglion. J Hand Surg [Am] 1985;10:697-703.
Kleinert HE, Kutz JE, Fishman JH, McCraw LH: Etiology and treatment of the so-called mucous cyst of the finger. J Bone Joint Surg 1972;54A:1455-8.
McEvedy BV: The simple ganglion: a review of modes of treatment and an explanation of the frequent failures of surgery. Lancet I 1956:135-136.
Nelson CL, Sawmiller S, Phalen GS. Ganglia of the wrist and hand. J Bone Joint Surg 1972;54A:1459-1464.
Richman JA, Gelberman RH, Engber WD, Salamon PB, Bean DJ: Ganglions of the wrist and digits: Results of treatment by aspiration and cyst wall puncture. J Hand Surg [Am] 1987;12:1041-1043.
Rizzo M, Beckenbaugh R: Treatment of mucous cysts of the fingers: Review of 134 cases with minimum 2-year follow-up evaluation. J Hand Surg 2003;28,3:519-524.
Soren A. Archives of Orthopaedic Trauma Surgery 1982;99,4:247-252
Soren A: Pathogenesis and treatment of ganglion. Clinical Orthopaedics 1963;48:173 179.
Watson, HK: Re-evaluation of the cause of the wrist ganglion. J Hand Surg 1989;14A,5:812- 817.
Young L, Bartell T, Logan SE: Ganglia of the hand and wrist. Southern Medical J 1988;81.6:751-760.
Zubowicz VN, Ishii CH: Management of ganglion cysts of the hand by simple aspiration. J Hand Surg [Am] 1987;12:618-620.